 Crohn’s disease (CD) is one of two inflammatory bowel diseases (the other being ulcerative colitis) that has become increasingly more prevalent in the U.S. over the past half century. It is estimated that 1.4 million Americans now currently have CD, making it a formidable chronic health burden to those who have it, and to our nation as a whole.1
Crohn’s disease (CD) is one of two inflammatory bowel diseases (the other being ulcerative colitis) that has become increasingly more prevalent in the U.S. over the past half century. It is estimated that 1.4 million Americans now currently have CD, making it a formidable chronic health burden to those who have it, and to our nation as a whole.1
Traditionally, CD has mostly affected populations of North America and Europe, but it’s now spreading across the globe.2 Places like Asia, Africa, and the Middle East are all seeing an increase in CD in their populations as they start to adopt a Western lifestyle signifying that environment, and not just genes, plays a major role in the development of this disease.
In this article, I will discuss what Crohn’s disease is and the risk factors associated with it. I will discuss treatment options in a future article.
What is Crohn’s Disease?
Crohn’s disease is an autoimmune disease that affects the gastrointestinal (GI) system. More specifically, it is a chronic, relapsing inflammatory disease that affects the GI system anywhere from the mouth to the anus.4 CD can also affect areas outside of the GI tract in rare instances.
At this time, CD is not curable and can only be put into permanent remission at best. Most patients will undergo a series of flare-up episodes and remissions alternating back and forth. Approximately 10%-15% of patients experience a chronic, continuous disease course with CD.5
The inflammation caused by CD usually occurs in the lining of the intestines. More often than not, it affects the very last 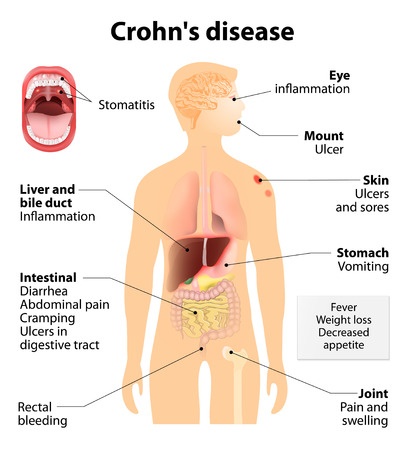 section of the small intestine called the ileum and also the large intestine (i.e. colon).6 The inflammation caused by CD can lead to a number of debilitating and painful symptoms. The list below is some of the more common ones:6,7
section of the small intestine called the ileum and also the large intestine (i.e. colon).6 The inflammation caused by CD can lead to a number of debilitating and painful symptoms. The list below is some of the more common ones:6,7
- Diarrhea
- Abdominal pain
- Fever
- Weight loss
- Reduced appetite
- Abdominal mass
- Anemia
- Blood or mucous in the stools
- Mouth sores
Anyone suffering from chronic diarrhea, abdominal pain, bloody stools, or unexplained fever or weight loss should see their doctor for evaluation. These may be a concern for CD or other gastrointestinal disorders.
CD may lead to abscesses, fissures, and/or fistulas in about one-third of patients.6 An abscess is a confined pocket of pus caused by an infection. A fissure is a crack or tear in the lining of the gastrointestinal tract. In CD, abscesses and fissures usually occur in or around the anal or rectal areas. A fistula is an abnormal connection or tunnel formed between two organs or body parts. CD patients can form fistulas between two different sections of their intestines or even between their intestines and their bladder, vagina, or surface of their skin.
Given the complications and damage CD inflicts on the GI tract, many patients will eventually need surgery to repair or remove parts of their intestines. Upwards of 70%-80% of CD patients will have required surgery by the 20-year mark.5 Greater than 10% of patients will require a permanent ostomy.
An ostomy is a small surgical opening formed in the abdominal wall to connect the portion of the intestine that remains to a small, pouch-like bag in order to collect fecal matter. Patients with an ostomy bag can no longer defecate and rely solely on this device to relieve themselves of their bathroom duties.
As you can see, the complications of CD can be serious, debilitating, and painful. These complications can have a major impact on a person’s psychosocial wellbeing. Many patients with CD will face challenges throughout their lifetime in terms of their academic pursuits, employment, personal relationships, and sexual health because of this.
Risk Factors For Crohn’s Disease
A single cause for CD has yet to be discovered and probably never will be. Instead, it appears that genetics, a dysfunctional immune system, disrupted gut microflora, and environmental factors, including diet, all contribute to the development of this chronic disease.
Role of Genetics in Crohn’s Disease
If any disease were 100% due to genes, then it would stand to reason that 100% of identical twins would be affected by the disease. This is called a concordance rate. In a European study looking at CD, identical twins had a concordance rate of only 20% to 50%.8 In non-identical twins the concordance rate was only 10%.
As you can see from these twin studies, CD is not entirely due to a person’s genetic makeup. Family history does play a limited role in CD though. Epidemiological studies have shown a 2% to 14% family history of CD in patients diagnosed with this disease.9 In addition, the lifetime risk of developing one of the inflammatory bowel diseases—CD or ulcerative colitis—in those with a first-degree relative with CD is 5%.8
Clearly, genes can play a role in the development of CD, but obviously other factors like the microbiome environment in the gut and diet play a part too. Let’s take a look at those next.
Role of Gut Microbiota and a Dysfunctional Immune System in Crohn’s Disease
The human body contains up to 100 trillion microorganisms in its gastrointestinal tract.10 These microorganisms are important in maintaining a healthy gut.
The GI tract contains “good” bacteria and “bad” bacteria. The good bacteria perform many valuable functions vital to maintaining a healthy gut. The bad bacteria can cause infections and other unwanted effects on the gut. Our good bacteria’s positive effects on the gut include the following:10,11
- Digestion and breakdown of non-digestible dietary fiber
- Production of certain vitamins and short-chain fatty acids
- Acts as a protective barrier against disease-causing bacteria (i.e. “bad” bacteria)
- Regulation of healthy immune system in the gut
When an imbalance occurs between these two types of bacteria, consequences develop. These include infectious diarrhea, inflammation of the lining of the intestines, and/or the dysregulation of our gut’s immune system.
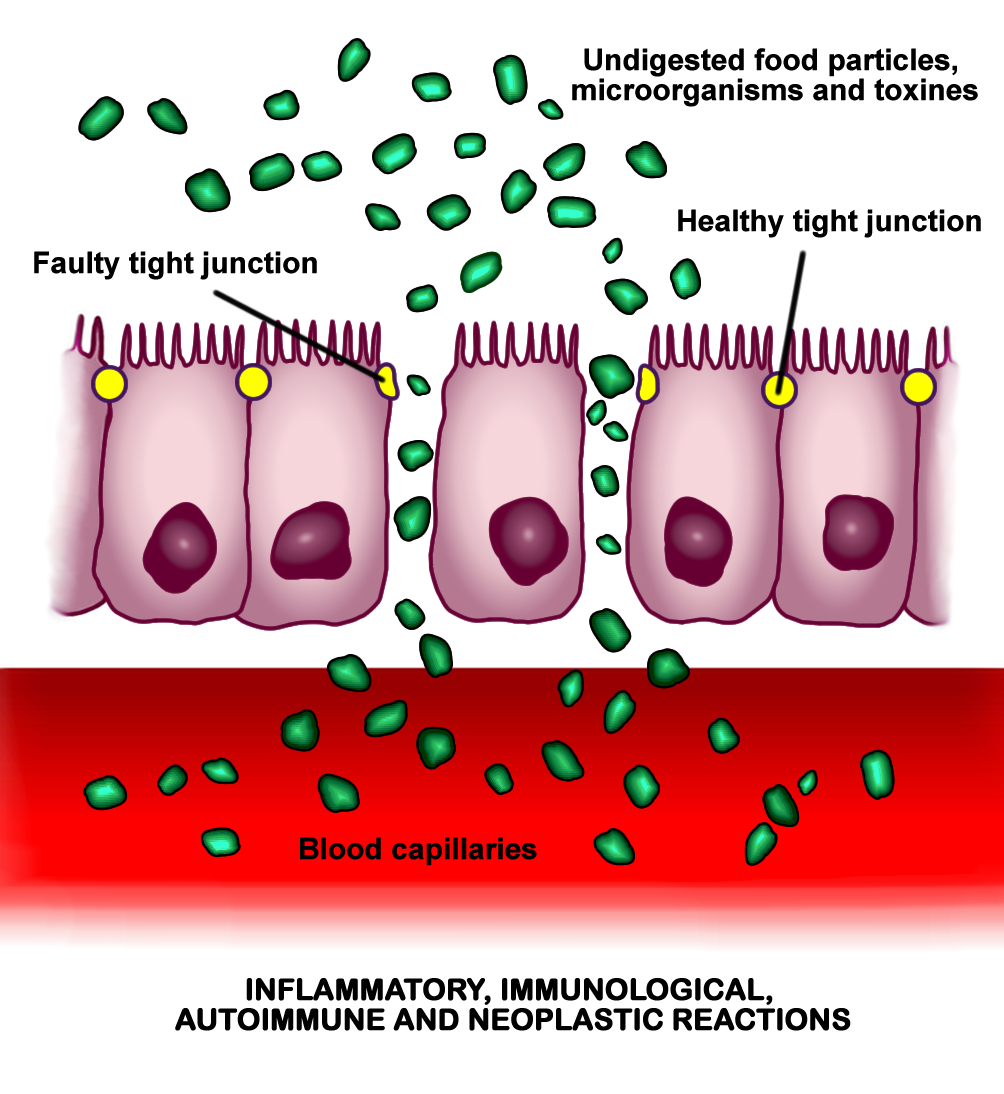 All of this can lead to or contribute to a “leaky” gut. A leaky gut occurs when the thin layer of cells lining the inside of the intestines is compromised. This thin layer of cells is responsible for absorbing nutrients and substances into our bloodstream from the foods we eat. This layer is only one cell thick. Normally, these cells line up tightly next to each other with little to no wiggle room in between. However, in inflammatory bowel disease the cells drift apart leaving gaps between each cell causing a “leaky” gut.12-14 As a result, substances like disease-causing viruses and bacteria and foreign proteins not normally absorbed into the bloodstream are now “leaking” through these gaps. This causes patients with CD to attack these substances leading to more inflammation and worsening of their disease and other inflammatory diseases.11
All of this can lead to or contribute to a “leaky” gut. A leaky gut occurs when the thin layer of cells lining the inside of the intestines is compromised. This thin layer of cells is responsible for absorbing nutrients and substances into our bloodstream from the foods we eat. This layer is only one cell thick. Normally, these cells line up tightly next to each other with little to no wiggle room in between. However, in inflammatory bowel disease the cells drift apart leaving gaps between each cell causing a “leaky” gut.12-14 As a result, substances like disease-causing viruses and bacteria and foreign proteins not normally absorbed into the bloodstream are now “leaking” through these gaps. This causes patients with CD to attack these substances leading to more inflammation and worsening of their disease and other inflammatory diseases.11
Role of Diet in Crohn’s Disease10
Diet plays a significant role in the development of CD. In fact, I would say it has the most important role in the development of CD.
The Western diet is implicated in higher incidences of inflammatory bowel disease. This is due to a higher fat content and lower fiber content of the diet, as well as a high consumption of animal protein in the diet.
Meat consumption in particular is associated with a higher incidence of CD. The more meat an individual consumes the higher their risk of developing CD. Meat includes all forms from beef, chicken, turkey, to pork. All of it can cause a problem in the development of CD.
A higher intake of refined sugars and processed carbohydrates like soda, desserts with added sugar, chocolate, and pastries have been implicated as a risk factor for CD. However, consumption of potatoes has actually been shown to reduce the risk of inflammatory bowel disease. This would make sense since potatoes are an unrefined plant food and naturally low in fat. Potatoes also contain a healthy dose of fiber. I always like to say it’s not the potato that’s the problem. It’s what you put on top the potato that will get you into trouble.
Patients with CD have a low intake of fiber, particularly from fruits and vegetables. Remember, fiber is only found in plant foods. In the Nurse’s Health Study a higher consumption of fiber from fruits and vegetables was shown to reduce the risk of CD. A Japanese health study showed that the consumption of fiber from fruits, vegetables, seaweed, dried mushrooms, and Japanese radishes was favorable in reducing patient’s inflammation levels too.
The bottom line is a diet with large amounts of whole, plant-based foods (i.e. fruits and vegetables) and low amounts of animal and processed foods is best in prevention strategies toward CD.
Role of Other Environmental Factors in Developing Crohn’s Disease10
Certain environmental factors can play a role in the development of CD. The first is smoking. Smoking doubles the risk of CD compared to nonsmokers. Smoking leads to more complications like fistula development and the need for surgery. Even secondhand smoke shows a similar effect on CD, although to a weaker degree than smoking directly.
Medication use can also affect CD risk. The chronic use of nonsteroidal anti-inflammatory drugs (i.e. aspirin, ibuprofen, naproxen, ketorolac) increases the risk of CD. The higher the dose and the longer a person takes them the more of a risk factor they become. This is thought to occur because anti-inflammatory medications can cause gaps to open between intestinal cells leading to a leaky gut. Oral contraceptives have been shown to increase the risk of CD, especially in women who also smoke. Finally, the early use of antibiotics in children can increase their risk of developing CD. It is thought this alters the gut microbiota and promotes inflammation. Responsible and conservative use of antibiotics in childhood should be the goal of every parent and pediatrician.
Vitamin D has also grabbed headlines regarding its role in CD. Many observational studies have shown lower blood levels of vitamin D in patients with CD.15 However, this does not mean that supplementing with vitamin D effectively treats CD. For this, we need interventional studies where CD patients are given vitamin D supplements and then followed for their effect on the disease. To date, there has only been a few small studies of this kind in humans. They have mixed results, some showing small positive effects during the short term, whereas others resulted in statistically non-significant results overall.16 Larger, more robust, interventional studies are needed to give us a better picture of vitamin D supplementation on CD before recommending this as a viable treatment option.
Other possible risk factors for the development or worsening of CD are air pollution, sedentary lifestyle, sleep disorders, ingestion of heavy metals such as mercury, a previous appendectomy, and stress, anxiety, or depression.
Summary
Crohn’s disease is a serious chronic illness affecting millions of people across the globe. Its effects can be debilitating and life changing, but they don’t have to be.
The best defense against CD is early detection followed by positive diet and lifestyle changes. Adopting a whole foods, plant-based diet is key to this. Simply receiving a diagnosis of CD without making diet or lifestyle changes will only guarantee a future of medications and surgery, all while continuing to battle this disease. Be good to your body and your body will be good to you. I will discuss dietary and medication treatment options in my next article on CD. Until then, eat plants, and the more the better.
Related article:
Crohn’s Disease – Diet vs Drug Treatment

.jpg) If you like what you see here, then you’ll LOVE my daily Facebook and Twitter posts! Also, don’t forget to sign up for my Free Online Mailing List to get all the latest updates from the Plant-Based Pharmacist!
If you like what you see here, then you’ll LOVE my daily Facebook and Twitter posts! Also, don’t forget to sign up for my Free Online Mailing List to get all the latest updates from the Plant-Based Pharmacist!
Check out my book, The Empty Medicine Cabinet, to start your journey towards better health. This step-by-step guide leads you through many of today’s common chronic diseases (heart disease, obesity, diabetes, cancer, and more), giving you the facts on food versus medication in treating these medical conditions. The book also contains an easy-to-follow guide on how to adopt a whole foods, plant-based diet as a part of an overall lifestyle change, producing the best possible health outcomes for you and your family. Hurry and get your copy today!
References:
1 Bandzar S, Gupta S, Platt MO. Crohn’s disease: a review of treatment options and current research. Cell Immunol. 2013 Nov-Dec;286(1-2):45-52.
2 Ponder A, Long MD. A clinical review of recent findings in the epidemiology of inflammatory bowel disease. Clinical Epidemiology. 2013;5:237-247.
3 Ye Y, Pang Z, Chen W, Ju S, Zhou C. The epidemiology and risk factors of inflammatory bowel disease. International Journal of Clinical and Experimental Medicine. 2015;8(12):22529-22542.
4 Baumgart DC, Sandborn WJ. Crohn’s disease. Lancet. 2012 Nov 3;380(9853):1590-605.
5 Cosnes J, Gower-Rousseau C, Seksik P, Cortot A. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011 May;140(6):1785-94.
6 Wilkins T, Jarvis K, Patel J. Diagnosis and management of Crohn’s disease. Am Fam Physician. 2011 Dec 15;84(12):1365-75. Review.
7 Ha F, Khalil H. Crohn’s disease: a clinical update. Therapeutic Advances in Gastroenterology. 2015;8(6):352-359.
8 Halme L, Paavola-Sakki P, Turunen U, Lappalainen M, Färkkilä M, Kontula K. Family and twin studies in inflammatory bowel disease. World Journal of Gastroenterology : WJG. 2006;12(23):3668-3672.
9 Liu JZ, Anderson CA. Genetic studies of Crohn’s disease: Past, present and future. Best Practice & Research Clinical Gastroenterology. 2014;28(3):373-386.
10 Legaki E, Gazouli M. Influence of environmental factors in the development of inflammatory bowel diseases. World Journal of Gastrointestinal Pharmacology and Therapeutics. 2016;7(1):112-125.
11 Babickova J, Gardlik R. Pathological and therapeutic interactions between bacteriophages, microbes and the host in inflammatory bowel disease. World Journal of Gastroenterology : WJG. 2015;21(40):11321-11330.
12 Schulzke JD, Ploeger S, Amasheh M, et al. Epithelial tight junctions in intestinal inflammation. Ann N Y Acad Sci. 2009 May;1165:294-300.
13 Zeissig S, Bürgel N, Günzel D, et al. Changes in expression and distribution of claudin 2, 5 and 8 lead to discontinuous tight junctions and barrier dysfunction in active Crohn’s disease. Gut. 2007;56(1):61-72.
14 Landy J, Ronde E, English N, et al. Tight junctions in inflammatory bowel diseases and inflammatory bowel disease associated colorectal cancer. World Journal of Gastroenterology. 2016;22(11):3117-3126.
15 Sadeghian M, Saneei P, Siassi F, Esmaillzadeh A. Vitamin D status in relation to Crohn’s disease: Meta-analysis of observational studies. Nutrition. 2016 May;32(5):505-14.
16 Masri OA, Chalhoub JM, Sharara AI. Role of vitamins in gastrointestinal diseases. World Journal of Gastroenterology : WJG. 2015;21(17):5191-5209.


Pingback: Crohn's Disease - Diet vs Drug Treatment – Plant Based Pharmacist