 In my last article on Crohn’s disease, I gave an overview of the disease along with things you can do to prevent it. In this article, I will discuss treatment options as it pertains to using diet versus medications.
In my last article on Crohn’s disease, I gave an overview of the disease along with things you can do to prevent it. In this article, I will discuss treatment options as it pertains to using diet versus medications.
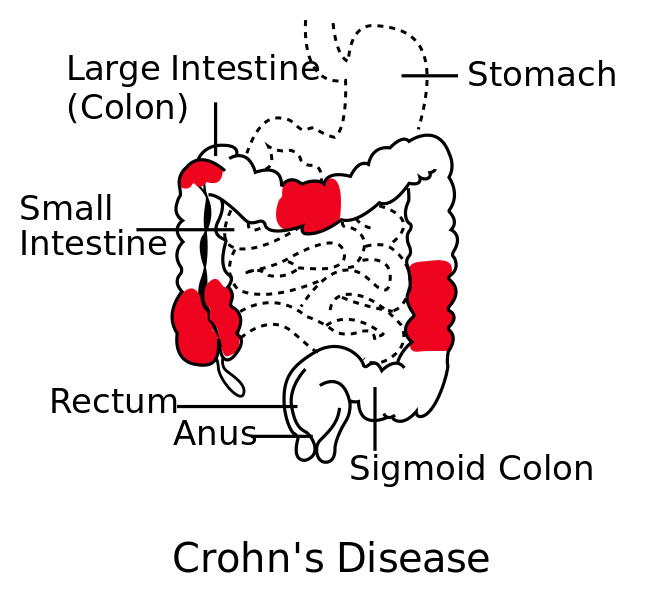
To provide a brief recap on Crohn’s disease, it is an autoimmune disorder resulting in a chronic, relapsing inflammatory process that affects the gastrointestinal system anywhere from the mouth to the anus.1 Crohn’s disease causes painful flare-ups which can lead to hospitalizations if severe enough. Patients often suffer from abdominal cramps, diarrhea (sometimes bloody), and painful ulcers/sores throughout their gastrointestinal tract. For a more detailed look into this disease please refer to my article – Crohn’s Disease – Overview and Diet & Lifestyle Connection.
Treating Crohn’s Disease with Diet
The bad news about Crohn’s disease is that it cannot be cured, not even with diet. The good news about Crohn’s disease is that it can be put into permanent remission if you adopt the correct diet. The earlier this dietary approach is taken the greater chance of success in putting this disease into remission.
Let me explain briefly the difference between curing a disease and putting a disease into remission. Curing a disease means you treat the disease and the disease goes away, forever. For example, you can cure an infection by treating it with antibiotics and killing the bacteria.
 Achieving remission with a disease involves treating the disease and putting it into a dormant state, resulting in the absence of disease activity. The disease is still there, and it can always rear its ugly head again, but it is not currently active while in remission. An example would be putting any of the autoimmune diseases, or even cancer, into remission with the hopes of it not coming back.
Achieving remission with a disease involves treating the disease and putting it into a dormant state, resulting in the absence of disease activity. The disease is still there, and it can always rear its ugly head again, but it is not currently active while in remission. An example would be putting any of the autoimmune diseases, or even cancer, into remission with the hopes of it not coming back.
With this being said, Crohn’s disease is best treated by adopting a diet that can put it into remission, instead of using drugs to simply manage the symptoms as they occur. A plant-based diet has been shown to be the most beneficial in doing this.2
There are observational studies showing a correlation between an increase incidence of Crohn’s disease and the consumption of junk foods and animal foods such as meat, dairy, and eggs.31 Likewise, observational studies show a decreased incidence of Crohn’s disease with the consumption of plant foods (i.e. fruits, vegetables).
While observational studies are nice, they do not prove direct cause and effect. They only show correlation. The best way to prove cause and effect is to conduct a human interventional study. These types of studies put patients on a specific diet (or drug) and then follow these patients to determine the outcomes that the interventions have on their disease over a course of time. Let’s take a look at interventional studies on diet and lifestyle and Crohn’s disease.
Crohn’s Disease Treated with a Semi-Vegetarian Diet
In 2010, an article published in the World Journal of Gastroenterology by Japanese medical doctors put patients on a plant-based diet to treat Crohn’s disease.3 This small study of twenty-two patients analyzed the effects of a semi-vegetarian diet on relapse rates of Crohn’s disease in a high-risk group of patients. The semi-vegetarian diet consisted of vegetables, fruits, legumes, potatoes, rice (mainly brown), miso soup, and green tea. Milk, eggs, and yoghurt (plain) were also included. Fish was served once a week, and meat once every two weeks.
The two-year study followed a total of sixteen compliant patients who continued their semi-vegetarian diet, and six non-compliant patients who reverted back to their omnivorous diet. At the 1-year mark, 100% of the semi-vegetarian group and just 33% of the omnivorous group remained in remission. At the 2-year mark, 92% of the semi-vegetarian group and only 16.7% of the omnivorous group remained in remission.
Clearly, a semi-vegetarian diet benefited significantly over an omnivorous diet in controlling this disease. This is the best interventional study to date that we have on diet and Crohn’s disease.
Crohn’s Disease Treated with Enteral Feedings
There have been successful interventional studies done with enteral feedings in Crohn’s disease.
[Note – Enteral feedings deliver a semi-thick liquid of calories and nutrients typically administered through a feeding tube to a patient. It replaces a diet of real food in patients who cannot eat actual food for whatever reason – maybe due to a hospitalization from a severe flare-up of Crohn’s disease.]
Studies of enteral feedings show a remission rate of about 80%-82%.4 However, patients are not likely to stay on this type of diet for long, as it is usually only used in the hospital setting or during severe flare-ups of Crohn’s disease.
Crohn’s Disease Treated with Carbohydrate-Specific Diets
Another small interventional study worth mentioning involved two groups of patients with Crohn’s disease, each group with 32 patients.5 The first group was given dietary advice to reduce consumption of refined sugars (sugar, white flour, white rice, etc.) and increase fiber intake by increasing fruit and vegetable consumption. The second group was given no dietary advice.
After a 52-month follow-up period, the group given advice to reduce refined sugars and increase fiber intake had less hospital admissions and less surgery than the group given no dietary advice.
Lastly, an important interventional study was performed over a 2-year period on patients with Crohn’s disease.6 This study consisted of 352 patients total, divided into two groups. Group A consisted of 162 patients. They were told to consume carbohydrates in their refined form (white flour, white rice, etc.) and to avoid unrefined carbohydrates (brown rice, whole grains, etc.). In addition, no limits were put on sugar intake in Group A. Basically, Group A was told to eat a diet of junk food.
Group B consisted of 190 patients. They were told to consume only unrefined carbohydrates high in fiber and to avoid all products containing sugar or white flour.
At the end of the study, the differences in sugar and fiber intake were clear and evident. Group A consumed high amounts of sugar and a low-fiber diet (junk food or “bad” carbs). Group B consumed low amounts of sugar and a high-fiber diet (healthy or “good” carbs). Surprisingly, no differences in clinical endpoints existed between the two groups.
Summary of Dietary Treatments in Crohn’s Disease
What we can take from these studies is that there is clear and distinct evidence that animal foods have a negative impact on Crohn’s disease. However, there is not clear-cut evidence that different types of carbohydrates (refined vs unrefined) have a major impact on the course of Crohn’s disease.
For these reasons, it would be in the best interests of Crohn’s disease patients to reduce or eliminate their consumption of animal foods as their first line of defense in putting this disease into remission. Avoiding processed carbohydrates may or may not be of any value after that. Adding in fruits, vegetables, and other high-fiber plant foods is beneficial in treating Crohn’s disease.
Treating Crohn’s Disease with Medications
 Despite the overwhelming evidence to use diet as the primary source of treatment in Crohn’s disease, most patients will be treated with medications in our healthcare system. The goals of drug therapy are to control symptoms, induce clinical remission, and maintain remission with minimal adverse effects.7
Despite the overwhelming evidence to use diet as the primary source of treatment in Crohn’s disease, most patients will be treated with medications in our healthcare system. The goals of drug therapy are to control symptoms, induce clinical remission, and maintain remission with minimal adverse effects.7
The hope with medication is to prevent or delay further deterioration of the patient’s condition with Crohn’s disease. Despite the widespread use of medication, up to 80% of Crohn’s disease patients will eventually require surgery to treat ongoing complications of their disease.8
Drug therapy typically involves using one or more of the following drug classes—prebiotics/probiotics, aminosalicylates, corticosteroids, thiopurines, methotrexate, biologic agents. All of these options act to either reduce inflammation or suppress the immune system.
If you remember, Crohn’s disease is an autoimmune disease involving the immune system. Modern drug therapy attempts to weaken our immune system to combat this, whereas proper dietary therapy strengthens our immune system in a healthy way. Therefore, medications come with side effects, while proper dietary therapy does not.
When discussing drug treatment options for Crohn’s disease, I will report success rates in terms of absolute risk reduction or numbers needed to treat (NNT). To understand what these statistical terms mean, please read my article – 3 Questions to Always Ask Your Doctor (or Pharmacist).
Prebiotics and Probiotics in the Treatment of Crohn’s Disease
Prebiotics and probiotics have been used to attempt to treat Crohn’s disease, but have been inconsistent or inconclusive in producing results.9 Lactobacillus GG may actually increase relapse rates in Crohn’s disease patients. Given this data, there are no current official recommendations encouraging the use of these products in Crohn’s disease.
Aminosalicylates in the Treatment of Crohn’s Disease
Mesalamine, sulfasalazine, balsalazide, and olsalazine make up this class of drugs used to treat Crohn’s disease. They are used in patients with mild disease activity.7
How they work: This class of drugs work by reducing inflammation in the intestinal tract.10
Success rates11
- 10% absolute risk reduction for inducing remission (NNT=10)
- 7.1% absolute risk reduction in maintenance of remission (NNT=14)
Adverse effects
Below are side effects for mesalamine, one of the more popular drugs within this class.12 To see side effects of other drugs in this class see the Medscape pages for sulfasalazine, balsalazide, and olsalazine.
Abdominal pain (4-8%)
GI discomfort (4-8%)
Headache (7%)
Flatulence (1-6%)
Nausea (1-6%)
Fatigue (3%)
Asthenia (3%)
Malaise (3%)
Weakness (3%)
Fever (3%)
Exacerbation of colitis (3%)
Dizziness (2-3%)
Rash (1-3%)
Pruritus (1-3%)
Acne (1-3%)
Corticosteroids in the Treatment of Crohn’s Disease
The corticosteroids include prednisone, prednisolone, methylprednisolone, and budesonide. They are only used for active flare-ups to induce remission in patients and should not be used long term. This is due to their inability to maintain remission, their severe, long-term side effects, and their problems causing patient dependency.13 The only exception to this is budesonide, which is prescribed for maintenance of remission in Crohn’s disease.
How they work: This class of drugs works by reducing inflammation in the intestinal tract.13
Success rates
- 33.3% absolute risk reduction for inducing remission with prednisone/prednisolone (NNT=3)11
- Budesonide has not been proven to be effective for the maintenance of remission in Crohn’s disease14
Adverse effects
The following side effects are for methylprednisolone, a drug commonly used in the hospital setting for treating severe flare-ups.15 To see side effects of other drugs in this class see the Medscape pages for prednisone, prednisolone, and budesonide. I have bolded long-term side effects of greatest concern and most likely to happen with this class of drugs.
(Note – Frequency not defined)
Acne
Amenorrhea
Delayed wound healing
Delirium
Diabetes mellitus
Edema
Emotional instability
Erythema
Fluid retention
GI perforation
Glucose intolerance
Growth suppression (children)
Hallucinations
Headache
Hepatomegaly
Hypokalemic alkalosis
Increased transaminases
Insomnia
Leukocytosis
Menstrual irregularity
Myopathy
Neuritis
Osteoporosis
Peptic ulcer
Perianal pruritus
Pituitary adrenal axis suppression
Protein catabolism
Pseudotumor cerebri (on withdrawal)
Psychosis
Sodium and water retention
Seizure
Tachycardia
Ulcerative esophagitis
Urticaria
Vasculitis
Vertigo
Weight gain
Thiopurines in the Treatment of Crohn’s Disease
The thiopurines consist of azathioprine and 6-mercaptopurine. These agents are typically used in the long-term maintenance of remission in Crohn’s disease and may be combined with corticosteroids and/or biologic agents.7 They take 3-6 months before becoming fully effective in the body.
How they work: The thiopurines act to suppress the immune system, leading to less inflammation in the gut over time.16
Success rates
- 20% absolute risk reduction in maintenance of remission (NNT=5)7
Adverse effects
This class of drugs has serious side effects to consider before taking. Eleven percent of individuals will stop taking these medications due to their adverse effects.17 The most serious of these includes Non-Hodgkin’s lymphoma, which occurs in 4 out of 10,000 patients who take these drugs.17 These drugs can also cause birth defects, so they should not be used during pregnancy or if planning to become pregnant.
The following side effects are for azathioprine. See the Medscape page of 6-mercaptopurine for its side effect profile.
Leukopenia (28-50%)
Infection (20%)
Lymphoma (< 1%)
(Note – Frequency not defined for side effects below)
Abdominal pain
Alopecia
Arthralgia
Bacterial, fungal, protozoal, viral infections
Bone marrow suppression
Diarrhea
Fever
Hepatotoxicity
Macrocytic anemia
Myalgia
Nausea or vomiting
Rash
Skin cancer
Steatorrhea
Sweet syndrome (acute febrile neutrophilic dermatosis)
Thrombocytopenia
Methotrexate in the Treatment of Crohn’s Disease
Methotrexate is used in the long-term maintenance of remission for patients intolerant to thiopurines.7 It also has some very severe side effects that must be considered before taking. Methotrexate should not be used in pregnancy or if you plan to become pregnant, as it can cause birth defects and fetal death.
Methotrexate is actually a chemotherapy agent used intravenously for cancer. However, for autoimmune diseases like Crohn’s disease it is used in its oral tablet formulation and taken by mouth. FYI – some of the side effects listed below are more relative to the intravenous form used to treat cancer.
How it works: Methotrexate works by suppressing the immune system, leading to less inflammation in the gut over time.19
Success rate
- 20% absolute risk reduction in maintenance of remission (NNT=5)7,11
Adverse effects20
>10%
Demyelinating encephalopathy with cranial irradiation or other systemic chemotherapy
Reddening of skin
Hyperuricemia
Ulcerative stomatitis
Glossitis
Gingivitis
Nausea and vomiting
Diarrhea
Anorexia
Intestinal perforation
Mucositis (dose-dependent)
Leukopenia
Thrombocytopenia
Renal failure
Azotemia
Nephropathy
Pharyngitis
1-10%
Alopecia
Photosensitivity
Rash
Abdominal distress
Malaise
Fatigue
Chills, fever
Decreased resistance to infection
Gastrointestinal hemorrhage
Myelosuppression
Disorders of lung, interstitial pneumonia (acute, chronic)
Atrophy of liver, cirrhosis, hepatic fibrosis or necrosis, elevated liver function tests, hepatic failure
Biologic Agents in the Treatment of Crohn’s Disease
The biologic agents are the big guns in the world of pharmaceutical treatments for autoimmune diseases. They are powerful drugs that target the body’s immune system and come with a side effect profile that definitely requires both patient and doctor to take a serious look at before using.
The biologic agents used in Crohn’s disease include infliximab, adalimumab, certolizumab pegol, and the newer agents natalizumab and vedolizumab. These agents are typically used in moderate to severe forms of Crohn’s disease, but are increasingly being considered during the early stages of the disease as well. In the absence of making dietary and lifestyle changes, biologic agents will be the cornerstone of lifelong therapy in most conventionally treated patients with Crohn’s disease.22
Anti-TNF Agents
The anti-TNF agents include infliximab (Remicade), adalimumab (Humira), and certolizumab pegol (Cimzia).
How they work: These agents work by suppressing the body’s immune system. More specifically, they target tumor necrosis factor α, a potent pro-inflammatory substance in the body that plays a pivotal role in the development of Crohn’s inflammation.21
Success rates
- 33.3% absolute risk reduction for inducing remission with 12-18 weeks of infliximab therapy (NNT=3)22
- 20% absolute risk reduction in maintenance of remission with 30-54 weeks of infliximab therapy (NNT=5)22
- 24% absolute risk reduction for inducing remission with 4 weeks of high-dose adalimumab therapy (NNT=4)23
- 39% absolute risk reduction in maintenance of remission with 56 weeks of adalimumab therapy (NNT=3)23
- Certolizumab pegol did not produce statistically significant results for inducing remission in Crohn’s disease24
- 8.3% absolute risk reduction in maintenance of remission with certolizumab pegol therapy (NNT=12)24
Adverse effects
This class of drugs has serious side effects to consider before taking them. Ten percent of patients will stop taking these medications due to their adverse effects.17 The most serious side effects include a lupus-like reaction (1%), serious infections (3%), and 6 out of every 10,000 people will develop cancer in the form of Non-Hodgkin’s lymphoma from taking these drugs.17
The side effects listed below are for infliximab.25 See the Mescape pages for the side effect profile of adalimumab and certolizumab pegol.
Development of antinuclear antibodies (50%)
Infection (36%)
Upper respiratory tract infection (32%)
Abdominal pain (26%)
Nausea (21%)
Infusion reaction (20%)
Headache (18%)
Development of antibodies to double-stranded DNA (17%)
Other respiratory infection (eg, sinusitis, cough) (12-14%)
Diarrhea (12%)
Elevated alanine transaminase (ALT; rarely >3 times upper limit of normal)
Bronchitis (10%)
Dyspepsia (10%)
Rash (1-10%)
Fatigue (9%)
Back pain (8%)
Rhinitis (8%)
Urinary tract infection (8%)
Arthralgia (1-8%)
Fever (7%)
Hypertension (7%)
Pruritus (7%)
Dyspnea (6%)
Candidiasis (5%)
Anti-Integrin Agents
Two newer biologic agents known as natalizumab (Tysabri) and vedolizumab (Entyvio) are currently approved by the FDA to treat Crohn’s disease. These medications are usually used after other drug therapies, including anti-TNF agents, have failed.
How they work: These drugs work by inhibiting the immune system. More specifically, they prevent white bloods cells from attaching to and entering cells on the inside surface of the intestines, preventing inflammation that would normally result from this process.26
Success rates
- 7% absolute risk reduction for inducing a response (but not a remission) after 10 weeks of therapy with natalizumab (NNT=14)27
- 18% absolute risk reduction in maintenance of remission after 36 weeks of natalizumab therapy (NNT=6)27
- 7.7% absolute risk reduction for inducing remission after 6 weeks of vedolizumab therapy (NNT=13)28
- 17.4% absolute risk reduction for maintenance of remission after 52 weeks of vedolizumab therapy (NNT=6)28
Adverse effects
This group of drugs has serious sides effects to consider before taking. The most severe of these occurs exclusively with natalizumab (but not vedolizumab). Natalizumab can cause a condition known as progressive multifocal leukoencephalopathy (PML), a serious infection of the central nervous system for which there is no specific treatment. PML occurs in 1 out of every 1,000 patients receiving natalizumab.29
The side effects listed below are for vedolizumab.30 See the Medscape page for natalizumab for its side effect profile.
Nasopharyngitis (13%)
Headache (12%)
Arthralgia (12%)
Nausea (9%)
Pyrexia (9%)
Upper respiratory tract infection (7%)
Fatigue (6%)
Cough (5%)
Bronchitis (4%)
Influenza (4%)
Back pain (4%)
Rash (3%)
Pruritus (3%)
Sinusitis (3%)
Oropharyngeal pain (3%)
Pain in extremities (3%)
Infections (0.85% per patient-year)
Infusion-related hypersensitivity (0.07%)
Serious infections (0.06% per patient-year)
Conclusion
As you can see, Crohn’s disease has many different treatment options available for patients. The safest and most effective of these are diet and lifestyle changes. Unfortunately, our current healthcare system only gives lip service to these approaches.
Most patients will only be offered drugs and surgery to treat their Crohn’s disease. It is important to understand the benefits and risks of taking medications before doing so if you choose this option.
No matter what approach you take to treating your Crohn’s disease make sure you become an informed healthcare consumer so you can make the best decision possible for you. There are no right or wrong decisions. There are only a different set of results depending on which choices you make.
Wishing you the best in your quest for health and happiness!
Related article:
Crohn’s Disease – Overview and Diet & Lifestyle Connection

If you like what you see here, then you’ll LOVE my daily Facebook and Twitter posts! Also, don’t forget to sign up for my Free Online Mailing List to get all the latest updates from the Plant-Based Pharmacist!
Check out my book, The Empty Medicine Cabinet, to start your journey towards better health. This step-by-step guide leads you through many of today’s common chronic diseases (heart disease, obesity, diabetes, cancer, and more), giving you the facts on food versus medication in treating these medical conditions. The book also contains an easy-to-follow guide on how to adopt a whole foods, plant-based diet as a part of an overall lifestyle change, producing the best possible health outcomes for you and your family. Hurry and get your copy today!
References:
1 Baumgart DC, Sandborn WJ. Crohn’s disease. Lancet. 2012 Nov 3;380(9853):1590-605.
2 Chiba M, Ohno H, Ishii H, Komatsu M. Plant-Based Diets in Crohn’s Disease. The Permanente Journal. 2014;18(4):94.
3 Chiba M, Abe T, Tsuda H, et al. Lifestyle-related disease in Crohn’s disease: Relapse prevention by a semi-vegetarian diet. World Journal of Gastroenterology : WJG. 2010;16(20):2484-2495.
4 Lee D, Albenberg L, Compher C, et al. Diet in the Pathogenesis and Treatment of Inflammatory Bowel Diseases. Gastroenterology. 2015;148(6):1087-1106.
5 Heaton KW, Thornton JR, Emmett PM. Treatment of Crohn’s disease with an unrefined-carbohydrate, fibre-rich diet. British Medical Journal. 1979;2(6193):764-766.
6 Ritchie JK, Wadsworth J, Lennard-Jones JE, Rogers E. Controlled multicentre therapeutic trial of an unrefined carbohydrate, fibre rich diet in Crohn’s disease. British Medical Journal (Clinical research ed). 1987;295(6597):517-520.
7 Wilkins T, Jarvis K, Patel J. Diagnosis and management of Crohn’s disease. Am Fam Physician. 2011 Dec 15;84(12):1365-75. Review.
8 Cosnes J, Gower-Rousseau C, Seksik P, Cortot A. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011 May;140(6):1785-94.
9 Manuc T-EM, Manuc MM, Diculescu MM. Recent insights into the molecular pathogenesis of Crohn’s disease: a review of emerging therapeutic targets. Clinical and Experimental Gastroenterology. 2016;9:59-70.
10 Punchard NA, Greenfield SM, Thompson RPH. Mechanism of action of 5-arninosalicylic acid. Mediators of Inflammation. 1992;1(3):151-165.
11 Bebb JR, Scott BB. How effective are the usual treatments for Crohn’s disease? Aliment Pharmacol Ther. 2004 Jul 15;20(2):151-9. Review.
12 Mesalamine Adverse Effects. Medscape. Available: http://reference.medscape.com/drug/asacol-hd-pentasa-mesalamine-342074#4. Accessed: 12 Dec 2016.
13 Irving PM, Gearry RB, Sparrow MP, Gibson PR. (2007), Review article: appropriate use of corticosteroids in Crohn’s disease. Alimentary Pharmacology & Therapeutics, 26: 313–329.
14 Kuenzig ME, Rezaie A, Seow CH, et al. Budesonide for maintenance of remission in Crohn’s disease. Cochrane Database Syst Rev. 2014 Aug 21;(8):CD002913.
15 Methylprednisolone Adverse Effects. Medscape. Available: http://reference.medscape.com/drug/medrol-medrol-dosepak-methylprednisolone-342746#4. Accessed 12 Dec 2016.
16 Neurath M. Thiopurines in IBD: What Is Their Mechanism of Action? Gastroenterology & Hepatology. 2010;6(7):435-436.
17 Siegel CA. Lost in Translation: Helping patients understand the risks of inflammatory bowel disease therapy. Inflammatory bowel diseases. 2010;16(12):2168-2172.
18 Azathioprine Adverse Effects. Medscape. Available: http://reference.medscape.com/drug/azasan-imuran-azathioprine-343191#4. Accessed 12 Dec 2016.
19 Egan LJ, Sandborn WJ. Methotrexate for inflammatory bowel disease: pharmacology and preliminary results. Mayo Clin Proc. 1996 Jan;71(1):69-80. Review.
20 Methotrexate Adverse Effects. Medscape. Available: http://reference.medscape.com/drug/trexall-methotrexate-343201#4. Accessed 12 Dec 2016.
21 Peake ST, Bernardo D, Mann ER, et al. Mechanisms of action of anti-tumor necrosis factor α agents in Crohn’s disease. Inflamm Bowel Dis. 2013 Jun;19(7):1546-55.
22 Bebb, J. R. and Scott, B. B. (2004), How effective are the usual treatments for Crohn’s disease?. Alimentary Pharmacology & Therapeutics, 20: 151–159.
23 Lichtenstein GR, Panaccione R, Mallarkey G. Efficacy and Safety of Adalimumab in Crohn’s Disease. Therapeutic Advances in Gastroenterology. 2008;1(1):43-50.
24 Nikfar S, Ehteshami-Afshar S, Abdollahi M. Is Certolizumab Pegol Safe and Effective in the Treatment of Patients with Moderate to Severe Crohn’s Disease? A Meta-analysis of Controlled Clinical Trials. Iranian Red Crescent Medical Journal. 2013;15(8):668-675.
25 Infliximab Adverse Effects. Medscape. Available: http://reference.medscape.com/drug/remicade-inflectra-infliximab-343202#4. Accessed 16 Dec 2016.
26 Singh H, Grewal N, Arora E, Kumar H, Kakkar AK. Vedolizumab: A novel anti-integrin drug for treatment of inflammatory bowel disease. Journal of Natural Science, Biology, and Medicine. 2016;7(1):4-9.
27 Sandborn WJ, Colombel JF, Enns R, et al. Natalizumab induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2005 Nov 3;353(18):1912-25.
28 Sandborn WJ, Feagan BG, Rutgeerts P, et al. Vedolizumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2013 Aug 22;369(8):711-21.
29 Guagnozzi D, Caprilli R. Natalizumab in the treatment of Crohn’s disease. Biologics : Targets & Therapy. 2008;2(2):275-284.
30 Vedolizumab Adverse Effects. Medscape. Available: http://reference.medscape.com/drug/entyvio-vedolizumab-999901#4. Accessed 18 Dec 2016.
31 Legaki E, Gazouli M. Influence of environmental factors in the development of inflammatory bowel diseases. World Journal of Gastrointestinal Pharmacology and Therapeutics. 2016;7(1):112-125.


.jpg)
Pingback: Crohn’s Disease – Overview and Diet & Lifestyle Connection