 Arthritis, including rheumatoid arthritis, is a growing and leading public health concern in many developed countries. In the United States, it’s the number one cause of disability, and its prevalence is rising due to the increase in obesity and age amongst the population [1]. In fact, data from the CDC found that 22.2% (49.9 million) adults age ≥ 18 had self-reported doctor-diagnosed arthritis. 42.4% of these arthritis sufferers reported limitations in their daily activity level because of the disease.
Arthritis, including rheumatoid arthritis, is a growing and leading public health concern in many developed countries. In the United States, it’s the number one cause of disability, and its prevalence is rising due to the increase in obesity and age amongst the population [1]. In fact, data from the CDC found that 22.2% (49.9 million) adults age ≥ 18 had self-reported doctor-diagnosed arthritis. 42.4% of these arthritis sufferers reported limitations in their daily activity level because of the disease.
Arthritis is also an expensive disease, costing a total of $128 billion annually in the United States [1]. Clearly, this chronic condition warrants serious attention in our efforts to prevent, limit, or even reverse the debilitating effects it has on individuals.
RHEUMATOID ARTHRITIS – WHAT IS IT?
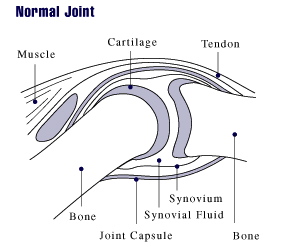
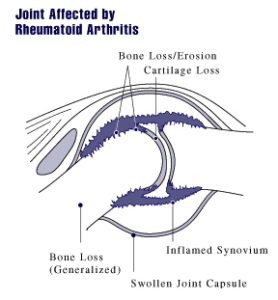
Rheumatoid arthritis (RA) is one of the most common forms of arthritis (osteoarthritis being the other) and is characterized by an autoimmune reaction affecting an individual’s joints [2]. This process results in tenderness, pain, swelling, and stiffness in the affected joint(s). Over time, chronic inflammation from RA can lead to destruction of tissue and bone in and around the joint resulting in permanent deformities. A continual reduction in one’s quality of life is typically seen as the disease progresses. Some patients with advanced disease even struggle to tie their own shoes or button their own shirt due to the severe pain it causes. Many individuals end up having to quit work and go on disability for the rest of their life. RA literally devastates those it affects.
RHEUMATOID ARTHRITIS – WHAT CAUSES IT?
It wasn’t until 1958 that the medical community had its first official criteria for the classification of rheumatoid arthritis [3]. This was preceded by the work of Dr. Charles Ragan, a rheumatologist, who first developed the test for rheumatoid factor, one of the key biomarkers present in 70-80% of patients with RA. Since then only one other biomarker has been discovered to ascertain the prevalence of RA in patients—anti-cyclic citrullinated peptide antibodies (anti-CCPs). Anti-CCPs are present in 50-70% of patients with RA and, like rheumatoid factor, are predictive of more serious cases of RA with a higher degree of future bone erosions [7]. Although having methods classifying the severity and prognosis of RA are useful, it does little good from a treatment aspect unless the cause of the disease is understood.
Over the decades following Dr. Ragan’s work much has been done to link RA with a genetic cause [4]. While it would be nice to blame everything on our genes current estimates suggests the risk of developing RA is only 50% determined by genes [5]. Even if one is genetically susceptible to developing RA it is also well established that an antigen (foreign protein or “toxin”) has to be presented to an individual’s immune system in order to trigger the cascade of events resulting in rheumatoid arthritis [3].
In other words, your genes play only a small role in whether or not you develop RA. Like many autoimmune diseases, RA is instead largely determined by environmental factors and how they interact with [and influence] the expression of your genes. Diet, smoking, and exposure to various infectious agents (viruses) have all been implicated as likely ‘triggers’ in the initiation process of RA [5,6]. Of these, diet is the major player and should serve as the cornerstone in any successful treatment program when treating RA. You’ll learn more about diet and RA later, but, first, let’s take a look at treating RA using the conventional route of medications.
RHEUMATOID ARTHRITIS – TREATMENT WITH MEDICATIONS
If you were to go to your doctor or other healthcare provider with a diagnosis of rheumatoid arthritis chances are you’ll quickly be introduced to a handful of medications. Conventional medicine has turned to pharmaceuticals as first line therapy to try and combat this chronic, debilitating condition. The goal of treatment is to reduce symptoms (pain, swelling, etc.) and delay progression of the disease through the use of various classes of medications. These include 5 classes of drugs—opioid pain relievers (used rarely) and 4 mainstays of treatment (NSAIDs, corticosteroids, DMARDs, and biological agents).
1) Opioids – (Codeine, Tramadol, Percocet, etc.)
- Aimed at reducing pain during short term (up to 6 weeks) but have no long term beneficial effects
- 18% of patients experienced improvement in pain [8]
- 30% of patients experienced one or more side effect (constipation, nausea/vomiting, dizziness, etc.) while taking opioids [8]
- Have the potential to become habit forming if taken long term
2) Non-steroidal anti-inflammatory drugs (NSAIDs) – Ibuprofen, Naproxen, Celebrex, etc.
- Aimed at reducing inflammation and pain during short term
- Do nothing to slow or halt progression of disease [9]
- Side effects include nausea, gastric distress/ulceration/bleeding, kidney damage, and increased risk of heart attacks/cardiac death [10]
3) Corticosteroids – Prednisone, Prednisolone, etc.
- Moderate to high dose therapy used short term to reduce inflammation and pain
- Low dose therapy used long term for its anti-inflammatory and immunosuppressive effects – delays progression of joint/bone erosion in clinical studies (often in combination with DMARD therapy) [11]
- Side effects remain a major concern for both patients and physicians
- Short term side effects include upset stomach, sleep disturbances, weight gain, and mood changes [12]
- Long term side effects include increased risk of osteoporosis, atherosclerosis, high blood pressure, Cushing’s syndrome, cataracts, glaucoma, stomach ulcers, and higher rates of infection due to suppressed immune system [12]
4) Disease-modifying antirheumatic drugs (DMARDs) – Sulfasalazine, Methotrexate, Hydroxychloroquine, Leflunomide, etc.
- Aimed at reducing inflammation and delaying progression of disease over long term
- Takes a minimum of 4-6 weeks to start working (Methotrexate); all other DMARDs take from 3-6 months to produce an effect [10]
- High long-term failure rates with DMARDs (insufficient clinical response or discontinuation due to toxicity or other reason) [13]
- Methotrexate (MTX) 2-year failure rate = 66% of patients
- Sulfasalazine (SSA) 2-year failure rate (patients previously failing on MTX) = 78% of patients
- Leflunomide 2-year failure rate (patients previously failing on SSA and MTX) = 87% of patients
- Hydroxychloroquine + MTX + SSA 2-year failure rate (patients previously failing on MTX + SSA) = 64% of patients
- 4 out of every 5 patients discontinue DMARD therapy within 5 years due to toxic side effects of the medications [14]
- Methotrexate side effects include damage to lining of stomach and intestines, headaches, confusion, blurred vision, mouth sores, hair loss, liver disease, blood cell disorders, severe lung damage, and increased risk of infections due to suppressed immune system [15,16]
- Side effects of other DMARDs can be found here
5) Biological Agents – TNF-α inhibitors (Humira, Enbrel, Remicade), IL-6 inhibitors, T and B Cell Inhibitors (Orencia, Rituxan)
- Aim to suppress immune and inflammatory processes occurring in RA patients
- Extremely expensive – average cost is $17,000-$18,000 per year. These medications show no current success in preventing long-term disability due to RA [17]
- Number of patients treated with biologics experiencing at least a 50% improvement in symptoms compared to placebo in clinical trials ranged from 9-36% depending on agent being used [18]
- Rare, but serious, side effects including increased risk of infections (including tuberculosis), cancer of the blood (lymphoma), and congestive heart failure can occur in those taking biological agents [19]
RHEUMATOID ARTHRITIS – TREATMENT WITH DIET
In contrast to drug treatment, it is very rare that the newly diagnosed patient with rheumatoid arthritis is offered a solution to their problem using nutrition. Being educated and trained as a clinical pharmacist, I was never taught about the link between diet and rheumatoid arthritis when I went through pharmacy school. Your doctors are likely to have been undereducated as well in these regards. Because of this, it isn’t surprising when I hear or meet patients and fellow medical professionals who think treating and evening reversing a serious autoimmune disease, like rheumatoid arthritis, with diet alone is just plain absurd. It is not. In fact, a switch to a whole foods, plant-based diet should be the first line of therapy offered to patients faced with this dreaded disease. The earlier this is done the better chance of halting and reversing the damage resulting from RA.
It was previously mentioned in the first part of this article that the introduction of foreign antigens (proteins or “toxins”) into the body is responsible for the antibody formation and inflammatory process taking place in RA. These antigens come in the form of food in many cases. One of the primary food sources for these foreign antigens is animal proteins (cow’s milk and meat) [20]. However, in some cases gluten (wheat protein) has also been found to act as a foreign protein capable of producing an autoimmune response in patient’s with RA [20].
Studies have shown that cow’s milk protein mimics proteins in our own body [21]. As a result, the antibodies created by our immune system towards the cow’s milk don’t just attack the cow’s milk protein (or other animal proteins), but they attack the tissues within the joints of RA patients as well. In essence, the body is literally attacking itself in its efforts to rid itself of the foreign proteins (antigens) consumed in the diet.
Another possible aggravating factor originating from the diet is the release of vasoactive amines (histamine, serotonin, octopamine, and phenylephrine) from various food sources [23]. These substances have been known to enhance the inflammatory process taking place in patients suffering from RA. Foods which have been link to this are pork, beef sausage, meat, tomato, spinach, shellfish, strawberries, chocolate, fish, coffee, alcohol, and citrus fruits [24].
As you can see, treating RA with medications will never target the true cause of disease. This is why removing animal-based proteins (milk, meat, and all dairy) is crucial for successfully treating this debilitating illness. Red meat, meat and meat products, and total protein content of the diet have all been shown to be significant risk factors for the development of inflammatory arthritis [22]. Eliminating animal products often does the trick in halting and reversing rheumatoid arthritis (as shown below in the video). If it does not do the trick for you then going on an elimination diet removing the remaining plant foods (citrus, tomato, wheat products, spinach, strawberries) may be something to consider. These plant foods can then be added back one at a time to see which ones cause troubling symptoms.
In the end it all starts with what you eat, not with the false promises of medications and prescription drugs that’ve shown a poor track record in treating RA. There is simply no downsides to adopting a whole foods, plant-based diet.
For more information on RA and diet read – Diet Therapy For The Patient With Rheumatoid Arthritis?
PATIENT STORIES – REVERSING RHEUMATOID ARTHRITIS
Check out Dustin Rudolph’s book The Empty Medicine Cabinet to start your journey towards better health. This step-by-step guide leads you through many of today’s common chronic diseases (heart disease, obesity, diabetes, cancer, and more), giving you the facts on foods versus medications in treating these medical conditions. The book also contains an easy-to-follow guide on how to adopt a whole foods, plant-based diet as a part of an overall lifestyle change, producing the best possible health outcomes for you and your family. Hurry and get your copy today!
23 Finn R. Pharmacological actions of food. In: Brostoff J, Challacombe SJ, eds. Food allergy and intolerance. London: Baillière Tindall, 1987:425–30.
24 Haugen M, Fraser D, Forre O. Diet therapy for the patient with rheumatoid arthritis? Rheumatology (Oxford). 1999 Nov;38(11):1039-44.



.jpg)
Im plant based now, but when I ate badly. I was diagnosed with heart failure, gout, fibromyalgia, very high blood pressure and was told I needed kidney surgery.
While Plant Based help all those things — still, only AFTER plant based did I get arthritis in my hands. Very troubling, and it hurts! Very much at night.
I stupidly started eating Dark Milk Chocolate because supposedly it helped overall inflammation– as told to me repeatedly by a dozen web sites.
It could be coincidence but after that I my hands hurt, then worse and worse. I met people who had same experience, online.,
If it caused inflammation there, it could easily and almost certainly causes it elswhere, including problems with heart, brain, kidneys.
I now realize DMC is very processed, and should have used very little and gone very slowly
Instead I dove into the deep end.
Now, t might take months, or longer, to check this out, by abstaining. This might now be a reoccuring thing, which will make my harder.
Do you know anything about dark milk chocolate and arthritis?
Yes, this study shows chocolate may cause issues for patients with arthritis – https://academic.oup.com/rheumatology/article/38/11/1039/1783279.